Summary
In
response to a formal request, the CRN has filed a formal critique of
California's Drug Medi-Cal (DM-C) program with the Legislative Analyst's
office in Sacramento. The critique concludes that DM-C has created a
system of care in California that is far below any standards of "Best
Practice" in the substance treatment field. Standards of care are
so low, the report suggests, that California is in violation of federal
Medicaid laws requiring that services be sufficient in amount, duration,
and scope to reasonably achieve their purpose
The report concludes
that "to conform to science-based principles and best practices,
DM-C coverage must be expanded for both adults and adolescents to include
reimbursement for residential services; day treatment; detoxification
(including standard detoxification medications); program-based case
management; clinically justified individual counseling; acupuncture
for acute and post-acute withdrawal, and services that are delivered
in community-based settings. Coverage for collateral services for family
members and 'significant others' must also be expanded to include individual
counseling, group counseling, and therapy."
Defining
the interest of the recovery community
The mission
of the Community Recovery Network (CRN) is to provide ongoing leadership
in community responses to alcohol and other drug (AOD) problems in California.
Drug Medi-Cal (DM-C) policies significantly impact community responses
to AOD problems. DM-C is important because many of those eligible for
the program - such as the severely mentally ill, persons with AIDS,
and recipients of public assistance, including minors - are disproportionately
impacted by substance disorders; additionally, DM-C Standards are often
used by Counties to define and govern non-DM-C treatment services to
avoid disparities in treatment and possible discrimination litigation.
Fiscal
imperatives for improving DM-C
Members of
our constituencies have expressed dismay at the enormous cost to the
citizens of California when AOD problems are not competently addressed.
The cost of these problems in the United States is estimated at $276
billion per year (NIDA/NIAAA,
1997). California's share of this cost, based on population, is
$35 billion. One could presume that a majority of that cost is imposed
by persons whose alcoholism or drug addiction is the most chronic and
severe, of which a disproportionate number are likely to be Medi-Cal
recipients.
Based on
prevalence estimates of 7.3% suggested by the most recent AOD survey
data (SAMHSA,
2002), we can estimate that the number of Californians in need of
treatment for chemical dependency is just under 2.5 million. In spite
of an often cited study by the State of California (DADP,
1994) showing that savings to taxpayers outpaced the public cost
of treating addicts by a 7-1 margin, California spends less than $600
million on treatment (CASA,
2001), adequate to treat just over 6% of those in need.
In a study
of the impact of untreated AOD problems on State governments conducted
by the Center for Substance Abuse at Columbia University (CASA,
2001), the percentage of California's State budget that is related
to AOD problems was estimated at 15.2%. Of that, only .4% was spent
on treatment, and the rest was spent on "shoveling up the wreckage"
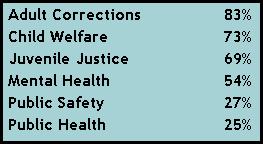
of untreated AOD problems. Portions of California departmental costs
related to AOD problems are estimated in the CASA study as follows:
Applying
only these percentages to California's 2002-03 budget, the cost to the
State of not adequately addressing alcohol and other drug problems is
$14.3 billion - over 14% of the total budget.
CRN's constituency
believes strongly that we cannot afford this luxury given California's
current fiscal shortfalls and deficits.
The
absence of effective management in the DM-C system
The Sobky
v. Smoley lawsuit in 1994 ended limits on utilization of DM-C by ruling
that drug treatment is an entitlement under Medicaid guidelines. In
response, utilization of outpatient and day treatment services increased
dramatically. There were no caps on rates, and reimbursement occurred
for clinic "visits" only, not for specific services. While
providers were required to have perfunctory "Utilization Review
Committees," ultimate decisions concerning both utilization of
services and the rates charged for those services were being made by
the service providers themselves without external regulations.
Interestingly,
an analogous problem was occurring in the private sector; hospital-based
chemical dependency treatment programs were charging private insurance
companies thirty to forty thousand dollars and more for thirty-day residential
programs, often with no limitations on the number of patient repeat
visits.
In short,
the chemical dependency service delivery system - both public and private
- had become a fiscal "runaway train."
While the
response in the private insurance sector was either strict managed care
practices or the elimination of chemical dependency benefits altogether,
the response of the DM-C system in 1996 was cost containment achieved
by constricted services such as limits imposed on rates and on the number
and kinds of services a client could access. The DM-C system appeared
- because of Sobky v. Smoley - unable to adopt the kinds of managed
care strategies that characterized other venues. The services received
by clients under DM-C, therefore, came not to be based on clinical guidelines
or recovery principles but rather on constrictions devised to contain
costs. These constrictions remain in place today.
Not only
are such constrictions without reference to our knowledge about successful
recovery, or to research-based clinical principles or science-based
treatment practices, but they sometimes frustrate the goals of other
State-sponsored services and result in far greater costs than those
that were "saved." For example, a chemically dependent pregnant
woman on the caseload of Child Protective Services will be eligible
for DM-C services during her pregnancy, but her eligibility will be
removed shortly after her child is born. With non-DM-C perinatal day
treatment services experiencing dramatic waiting lists in many Counties,
this can result in substance relapse, loss of custody of the child,
and the ultimate failure of family reunification. Or a chemically dependent
severely mentally ill person who is in need of comprehensive residential
treatment will find that it is not a covered Medi-Cal benefit and hence
unavailable in the County, resulting in psychiatric emergency. In these
cases, the "cost containment" measures result in costs to
the State that are far greater than those of treatment, such as out-of-home
foster care placement and exorbitant psychiatric emergency services.
Not surprisingly,
these "cost containment" measures in 1996 were soon followed
by the elimination of State mandates for providers to perform the monthly
utilization review that had provided the only mechanism of outside monitoring
of quality assurance in the system. Although an annual Utilization Review
mechanism was to have been instituted by the State, this has occurred
only sporadically, and the only specific control on provider utilization
of DM-C is the occasional and expensive provider audit.
"Moderate
Treatment" and Best Practices
Prior to
Sobky v. Smoley, the DM-C system was presented in theory as a program
for treating only "moderately impaired" chemically dependent
persons. Those severely impaired were to be referred elsewhere, presumably
to residential treatment facilities in those Counties where such services
were available. The system still carries that presumption. The problem
is that Sobky v. Smoley cannot be interpreted to apply solely to chemically
addicted individuals who are "moderate users." Indeed, all
persons who are diagnosed with chemical dependency and who are Medi-Cal
eligible are entitled to treatment that meets reasonable "best
practices" standards. DM-C, however, does not reimburse for services
and interventions of a variety and at a frequency that would conform
to the principles governing best practices and science-based treatment
of substance disorders such as those defined by the National Institute
on Drug Abuse's "Principles
of Drug Addiction Treatment" (NIDA, 1999) and by the Center
for Substance Abuse Treatment's "TIPS,"
(CSAT, 2002). California's DM-C program indeed appears to be in violation
of 42
USC 1396a(a)(10)(B), which states that "… service(s) must
be sufficient in amount, duration, and scope to reasonably achieve (their)
purpose (and) the Medicaid agency may not arbitrarily deny or reduce
the amount, duration, or scope of a required service ... to an otherwise
eligible recipient solely because of the diagnosis, type of illness
or condition."
To conform
to science-based principles and best practices, DM-C coverage must be
expanded for both adults and adolescents to include reimbursement for
residential services; day treatment; detoxification (including standard
detoxification medications); program-based case management; clinically
justified individual counseling; acupuncture for acute and post-acute
withdrawal, and services that are delivered in community-based (sic.
non-clinical) settings. Coverage for collateral services for family
members and "significant others" must also be expanded to
include clinically justified individual counseling, group counseling,
and therapy.
Legislation
has been introduced in the past to adapt DM-C to the "rehab model"
utilized by the Mental Health system, adding many of the benefits described
above. While few would argue that it is acceptable for the regulations
governing public treatment for chemical dependency in California to
be below standards of best practice, it will be difficult for the DM-C
program to achieve best practices standards unless it also incorporates
realistic monitoring and management mechanisms that prevent abuse of
the system. Unlike Short-Doyle Medi-Cal reimbursement for mental health
services, AOD services for Medi-Cal recipients are still defined as
an entitlement under federal Medicaid guidelines by Sobky v. Smoley.
Extending reimbursed services to include case management, residential,
and other services, is therefore not politically feasible unless there
are intelligent mechanisms in place to manage the costs and utilization
of this entitlement. These mechanisms are allowed under 42 USC 1396a(a)(10)(B),
as follows: "The agency may place appropriate limits on a service
based on such criteria as medical necessity or on utilization control
procedures." In order to achieve this, the State Alcohol and Drug
Program will need to obtain a Federal Medicaid Managed Care waiver from
the Center for Medicare & Medicaid Services.
The CRN also
urgently proposes an extension of the DM-C benefit for women under the
jurisdiction of Child Protective Services who have lost custody of their
children for reasons relating to their chemical dependency when family
reunification is the ultimate goal. Restrictions could be placed on
this extension, such as a requirement to comply with the chemical dependency
treatment plan.
Distinguishing
Characteristics of Substance Disorders
There is
another systemic problem with the DM-C program. Medi-Cal in general
has evolved to provide reimbursement mechanisms for the treatment of
physical illnesses. While alcoholism and drug addiction have been identified
by the medical and research communities as diseases, three very significant
factors distinguish substance disorders from other diseases. These three
factors must be systemically addressed in order to optimize successful
outcomes in any system of care.
- Persons
with other illnesses generally seek medical care when their condition
becomes symptomatic. This is not true of persons with substance disorders
due to the stigma, denial, hopelessness, impaired judgment, and other
issues associated with AOD problems.
- While
certain other medical interventions require a period of rehabilitation
that involves non-medical services, and while certain other chronic
diseases require behaviors or actions on the part of the patient in
order for the disease to remain in remission, long term recovery from
substance disorders uniquely depends in most cases upon ongoing, patient-initiated
activities and involvement with non-professional community resources
(e.g. peer-support groups).
- Persons
with substance disorders - particularly in cases where the condition
has progressed to the degree that public sector services are required
- typically have concomitant public health, mental health, and social
issues whose resolution is tantamount to substance recovery and which
must therefore be thoughtfully incorporated into the AOD treatment
continuum.
These three
distinctions suggest a critical need for comprehensive case management
services (currently not a covered benefit under DM-C). But the recovery
community's collective experience with successful recovery, as well
as the need for quality assurance and cost effectiveness within the
DM-C system, suggests that traditional case management as utilized in
the health and mental health systems of care may not adequately or appropriately
address all of these unique characteristics of substance disorders.
The
Solution
Based on
the problems we have described so far, it may be concluded that the
solution to improving the DM-C program must, at a minimum, include the
following:
- Services
must be reimbursed that conform to research-based treatment principles
and best practices. While Sobky v. Smoley prohibits the State from
discriminating about who becomes DM-C certified, it does have the
authority to establish the clinical standards under which all providers
must operate their treatment services. Guidelines should include,
at a minimum, those defined by the National Institute on Drug Abuse's
"Principles
of Drug Addiction Treatment" (NIDA, 1999) and by the Center
for Substance Abuse Treatment's "TIPS,"
(CSAT, 2002), including especially, for adolescent treatment services,
TIP 31: "Screening and Assessing Adolescents For Substance Use
Disorders," and TIP 32: "Treatment of Adolescents With Substance
Use Disorders," and the formal adolescent
treatment guidelines developed by California's Department of Alcohol
and Drug Programs (2002)
- The DM-C
system must have intelligent mechanisms governing the authorization
and utilization of services. Such management requires fundamentally
that the decisions made about what services are appropriate to an
individual client at what stage in his or her recovery and at what
frequency need to be made by an entity other than the one that will
provide the service and receive the reimbursement. These decisions
also need to be made by an entity that is neutral to local political
agency or "turf" issues to assure that utilization decisions
are based to every extent possible upon what services will most likely
result in the client's successful recovery.
- Mechanisms
need to be built into the system of care to enhance long term recovery
as opposed to simply encouraging people to enter treatment. Some administrators
believe that the greatest current cost burden on the treatment system
is not the individual who is a success and who therefore heavily utilizes
services for a long period of time, but rather the failures - those
individuals who access the system again and again but who never achieve
recovery.
While our
critique has made specific references to the problems of the DM-C program,
it is difficult to develop realistic and comprehensive solutions to
these problems without considering the overall response to AOD problems
at the County level. As has been noted, DM-C guidelines are used in
many Counties to set standards of care for non-DM-C treatment services.
Conversely, in other Counties, DM-C has resulted in a "2-tier"
system where Medi-Cal eligibility influences a person's qualification
for certain services. Less restrictive Net Negotiated Amount (NNA) funding
is able to fund a scope, duration and intensity of service which is
more appropriate clinically. It is not possible for clients of programs
funded solely by DMC to receive the same level of treatment that a client
can get in a program funded by NNA or NNA + DM-C.
It is the
strong belief of the CRN that the quality, consistency, appropriateness,
and timeliness of services received by residents of any County should
not be dictated by any status. When someone residing in a County has
an alcohol or other drug problem, the case can be made - financially,
ethically, and morally - that it is in the vital interest of that County
(and hence of the State) to respond to that problem with dispatch, and
to dedicate any and all resources necessary until successful recovery
for that individual is achieved. Failure to do so inevitably results
in enormous emotional costs to the person themselves and to their family,
friends, and loved ones, as well as lost productivity and colossal costs
to taxpayers for criminal justice, public health, and social services.
So, while
it may be beyond the scope of the Legislative Analyst's current investigation,
the CRN believes that any recommendations to the legislature concerning
DM-C should be ultimately viewed in the context of the entire AOD system
of care. The last effort by the State to address comprehensive system
of care issues deteriorated into a recommendation for modifications
in data collection (LAO,
1999).
An
Independent, Entry Level, Recovery Advocacy System in Each County
CRN proposes
the creation in each County (and in representative regions for Counties
with populations under 30,000) of a "Recovery-Based Case Management
System." The system would be operated under contract with the State
or County by a private entity who was not a DM-C or treatment service
provider, and who would perform the following functions:
- A 24-Hour
per day drug hotline and response team. Any private citizen residing
in the jurisdiction, or any professional such as a physician or therapist,
or any public employee such as a probation or parole officer, public
health or social service worker, could access the response team with
a single phone number. The team from which the person responding would
be selected would represent the diversity of the jurisdiction to assure
cultural and linguistic competence in the response. Requirements for
all response team members, who would work under clinical supervision,
would include (a) an Alcohol and Drug Counseling Certificate or its
equivalent; (b) competence in addiction severity assessment, family
interventions, brief crisis counseling, and motivational interviewing,
and (c) comprehensive knowledge of all community service providers,
including knowledge of all means by which people achieve and maintain
recovery from AOD problems, and of the community resources relative
for each.
- Comprehensive
and mobile case management services. The assigned Response Team member
would assess the individual referred to the system and the environment
in which they are functioning and work to remove any barrier to successful
recovery for both the individual and the family members. The person
would also authorize services within the formal treatment provider
network of the County for both the individual and his or her family
members, and would assist the client in accessing ancillary (non-treatment)
services that are deemed important to support the persons long term
recovery (such as mental health, public health, and vocational and
other services, and safe housing). These persons would operate in
conjunction with law enforcement, Mental Health crisis teams, social
workers, and others who encounter people with AOD problems in the
community
Recovery
Advocacy in the AOD treatment system is not an unprecedented concept.
Many drug court venues in California and around the country have adopted
a "Court Liaison" function - a person who mediates between
the court, probation, and treatment system on behalf of the client or
offender. The role of the Liaison is to assess and explain options to
the client, to propose referral recommendations to the drug court judge,
and then to "leave no stone unturned" in assuring that the
client is successfully engaged and retained in the recommended services.
Many Counties in California adopted a similar "recovery advocacy"
model for their perinatal case management services, and similar case
management services were successfully provided to SSI recipients before
the elimination of the alcoholism and drug addiction disability benefit.
The recovery
community has learned that not everyone with AOD problems needs formal
treatment. For many people, 12-Step and faith-based activities and their
equivalent, which may or may not be in combination with clean and sober
housing, are adequate for successful recovery. The proposed system would
be distinguished from traditional case management services that are
used in the public and private health sector in that their primary objective
would not be exclusively clinical (e.g. to access clinical services),
but to assist the client in engaging in those natural community supports
that enable long term recovery.
Based upon
the 2.5 million Californians who are estimated to be severely impacted
by alcohol and other drug problems, the cost of such a Recovery-Based
Case Management system, with an average case load of 70 persons, could
be estimated at $1.5 billion. However, this system should not be construed
as supplanting the significant need for additional treatment resources.
Indeed, the system's effectiveness would be severely compromised if
implemented in the current environment of resource-scarcity and substandard
services.
What
would a Comprehensive Treatment System Cost?
If California
were to invest in a comprehensive infrastructure to provide in each
County a realistic and effective response to alcohol and other drug
problems, the cost would depend significantly upon whether or not the
State is able to enact effective "Substance Abuse Parity"
legislation. This is because an estimated 75% of persons needing treatment
or recovery support services are in the work force (SAMHSA, 1999), and
many of these individuals are privately insured. A relatively weak parity
bill (SB599) was passed last year, but was withdrawn under threat of
veto by the Governor.
Using an
average treatment cost of $5,000, what might a comprehensive treatment
and recovery infrastructure for California require in terms of a public
investment? Of the 2.5 million needing recovery, we would estimate that
70% would either (a) require recovery support only (with no formal treatment),
or (b) be able to self-pay for treatment, or (c) be privately insured.
This portion of the 2.5 million people would therefore require no public
investment unless the State is unable to enact private insurance parity
legislation. Then the investment required for this group is estimated
at $3.5 billion.
We would
estimate the remaining 30% of the population as follows:
| |
Percentage |
Number |
Investrment |
| Uninsured
and requiring public treatment |
12% |
300,000 |
$1,500,000,000
|
| Eligible
for Medi-Cal (includes Federal match |
18% |
450,000 |
$2,000,000,000
|
| Recovery-Based
Case Management System |
|
|
$1,500,000,000
|
| Current
Investment |
|
|
($600,000,000) |
| Total
Infrastructure Investment: |
|
|
|
|
With Private Insurance Parity |
|
|
$4,400,000,000
|
| Without
Private Insurance Parity |
|
|
$7,900,000,000
|
Two things
are important to note when considering this investment:
- Unlike
the $35 billion that Californians are currently spending each year
on untreated AOD problems, this investment is not a continuing annual
cost. As people with severe alcohol and other drug problems begin
to successfully recover as the result of this investment, the cost
of maintaining the infrastructure declines dramatically.
- This estimated
cost (like California's
proposed $9.9 billion high speed train) should be viewed not as
an added cost but as a long-term investment. Currently, any
fiscal impact of the AOD treatment investment dollars cannot be measured
because the investment is so small. For example, the $120 million
invested in treatment as a result of the Substance Abuse and Crime
Prevention of 2000 (Proposition 36) - even under the sub-standard
treatment provided by the current system - is adequate to treat less
than 11% of the chemically dependent persons who are involved with
the criminal justice system, and less than 2.5% of the total population
who are in need of treatment or recovery support services. Therefore,
even success rates that are far above average will have a negligible
impact on the overall cost of criminal justice services in the State.
The comprehensive infrastructure suggested, however, even with lower
than average success rate, would reduce the current $14.3 billion
cost to the State to just over $4 billion in ten years.
CRN's
Recommendations
In summary,
the CRN recommends:
- That application
be made for a Managed Care waiver from the Center for Medicare &
Medicaid Services.
- That the
State Plan be amended to implement the "Rehab option" for
AOD services.
- That the
California Department of Alcohol and Drug Programs assemble stakeholders
including County Alcohol and Drug Program Administrators, representatives
of the recovery community, and providers, to address strategic issues
concerning the design of the Recovery-Based Case Management System.
Sources
Cited
CSAT, 2002,
Treatment Improvement Exchange, Treatment
Improvement Protocols (Best practice guidelines for the treatment
of substance abuse).
Department
of Alcohol and Drug Programs (1994), State of California, "Evaluating
Recovery services: The California Drug and Alcohol Treatment Assessment."
1700 K Street, Sacramento, CA 95814.
Department
of Alcohol and Drug Programs (2002), State of California, "Youth
Treatment Guidelines." 1700 K Street, Sacramento, CA 95814.
Legislative
Analyst's Office (July 13, 1999), "Services
Are Cost-Effective to Society Substance Abuse Treatment in California,"
LAO Publications, 925 L Street, Suite 1000, Sacramento, CA 95814.
CASA (January,
2001). "Shoveling
Up: The Impact of Substance Abuse on State Budgets." National
Center on Addiction and Substance Abuse at Columbia University.
National
Institute on Drug Abuse/National Institute on Alcohol Abuse and Alcoholism
(1998), The
Economic Costs of Alcohol and Drug Abuse in the United States, U.S.
Government Printing Office, Washington, DC, 1998.
NIDA, 1999.
Principles of
Drug Addiction Treatment: A Research-Based Guide. National Institutes
of Health, U.S. Department of Health and Human Services.
SAMHSA, 1998
(1998 National Household Survey on Drug Abuse), U.S. Department of Health
and Human Services. Rockville, MD.
SAMHSA, 2002
(2001 National
Household Survey on Drug Abuse), U.S. Department of Health and Human
Services. Rockville, MD.
|
|